COVID-19 has affected millions of people worldwide, leaving many with long-term symptoms, such as fatigue, shortness of breath, and cough. For people who had COVID-19, there is growing concern about the development of asthma as a long-term complication. In this article, we will discuss whether COVID-19 can lead to asthma and the possible underlying mechanisms.
Understanding Asthma
Asthma is a chronic respiratory disease that affects the airways in the lungs. The airways become inflamed, swollen, and narrow, making it difficult to breathe. This condition affects people of all ages and can range from mild to severe.
Symptoms
The most common symptoms of asthma include:
Wheezing: A high-pitched whistling sound when breathing.
Shortness of Breath: Difficulty catching your breath or feeling like you cannot get enough air.
Chest Tightness: A feeling of tightness or pressure in the chest.
Coughing: A persistent cough, especially at night or early in the morning.
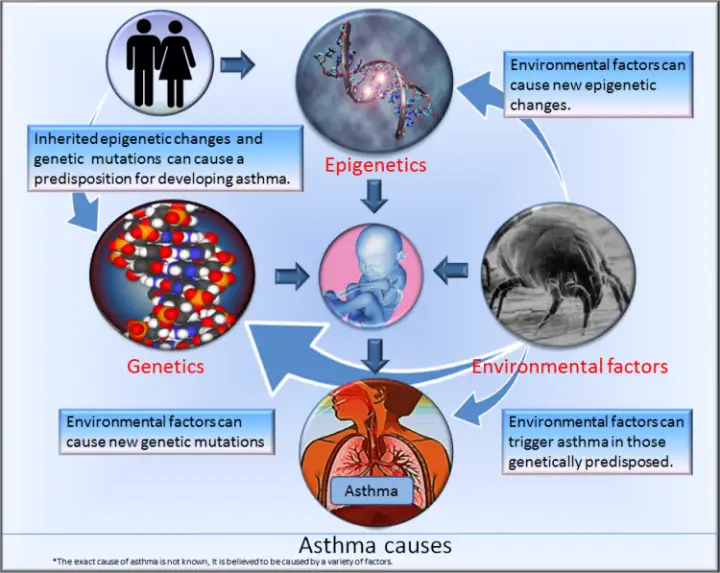
Causes
Asthma is caused by a combination of genetic and environmental factors. People with a family history of asthma are more likely to develop the condition. Additionally, exposure to certain triggers can cause or worsen asthma symptoms. These triggers include:-
Allergens: Dust mites, pollen, pet dander, and mold can trigger asthma symptoms in some people.
Respiratory Infections: Viral infections, such as colds and the flu, can cause asthma symptoms.
Air Pollutants: Pollution, smoke, and fumes from chemicals can irritate the airways and cause asthma symptoms.
Exercise: Physical activity can trigger asthma symptoms, especially in people with exercise-induced asthma.
Diagnosis
To diagnose asthma, your healthcare provider will perform a physical exam and review your medical history. They may also perform lung function tests to measure how well your lungs are working. These tests may include:-
Spirometry: A test that measures how much air you can breathe in and out, and how quickly you can exhale.
Peak Flow Test: A test that measures how much air you can exhale forcefully.
Methacholine Challenge Test: A test that measures how sensitive your airways are to a specific trigger.
Treatment
There is no cure for asthma, but treatment can help control symptoms and improve lung function. Treatment may include:-
Inhalers: Medications that deliver medicine directly to the lungs to reduce inflammation and relax the airways.
Allergy Medications: Antihistamines, decongestants, and corticosteroids can help reduce the symptoms of allergies that trigger asthma.
Immunotherapy: Allergy shots can help reduce the body’s reaction to specific allergens over time.
Lifestyle Changes: Avoiding triggers, quitting smoking, and maintaining a healthy weight can help manage asthma symptoms.
Can COVID-19 lead to Asthma?
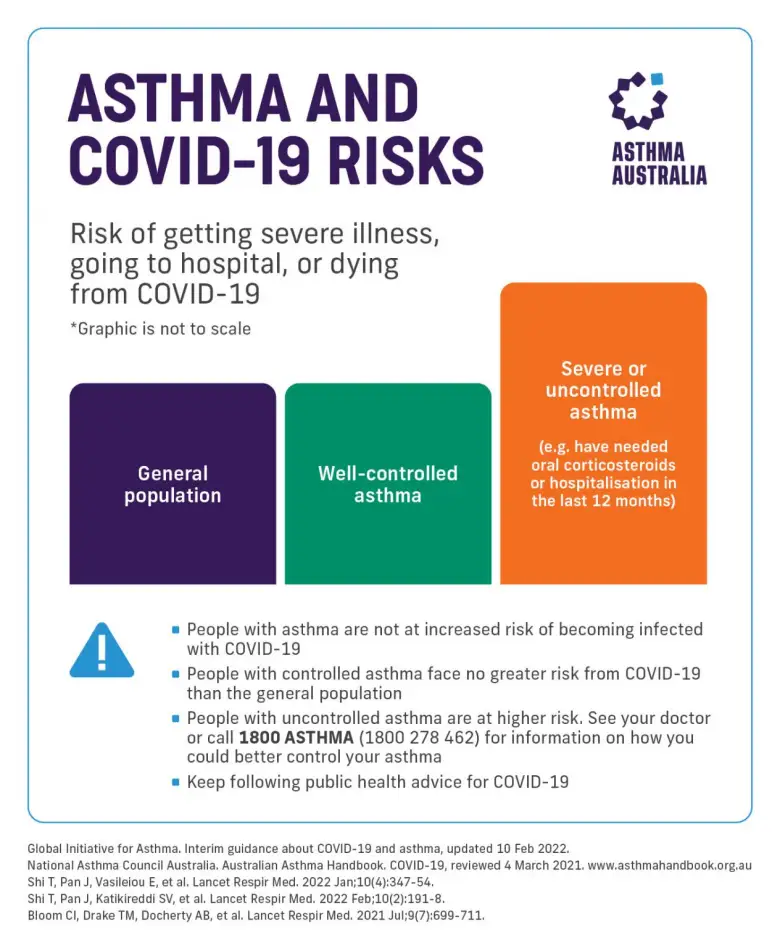
While COVID-19 primarily affects the respiratory system, it is not known to directly cause asthma. However, COVID-19 can cause significant lung damage and inflammation, which may lead to respiratory symptoms that mimic asthma. COVID-19 can also trigger asthma symptoms in people who already have asthma.
Studies have shown that some people who had COVID-19 experienced new or worsening respiratory symptoms, including shortness of breath and wheezing, which are hallmark symptoms of asthma. These symptoms can persist even after recovery from COVID-19, leading to a potential asthma diagnosis. A study published in The Lancet Respiratory Medicine found that 1 in 5 people who had COVID-19 experienced new or persistent respiratory symptoms, which can lead to a diagnosis of asthma.
Underlying Mechanisms
The exact mechanisms behind the link between COVID-19 and asthma are not yet fully understood. However, it is believed that the virus can cause damage to the airways and lungs, leading to inflammation and scarring. This damage can persist even after recovery from COVID-19 and may lead to asthma-like symptoms. Additionally, COVID-19 can trigger an immune response that causes inflammation, which can also lead to asthma symptoms.
Preventing Asthma after COVID-19
While it is not possible to prevent the development of asthma after COVID-19, there are steps people can take to reduce their risk. These include:
- Following up with a healthcare provider after recovery from COVID-19
- Maintaining a healthy lifestyle with regular exercise and a balanced diet
- Avoiding triggers such as smoking and exposure to pollutants
- Monitoring respiratory symptoms and seeking medical attention if they persist
Factors that Impact the Severity of Damage to the Lungs
The lungs play a crucial role in the respiratory system by delivering oxygen to the body and removing carbon dioxide. However, they are susceptible to damage from various factors, such as infections, pollutants, and smoking. The severity of damage to the lungs can vary based on several factors. In this article, we will discuss the factors that impact the severity of damage to the lungs.
Age
Age plays a significant role in the severity of lung damage. As we age, our lungs lose elasticity, and the air sacs can become damaged, leading to a reduction in lung function. Older adults may experience more severe lung damage from respiratory infections such as COVID-19.
Smoking
Smoking is a leading cause of lung damage. The toxins in cigarette smoke can cause inflammation, scarring, and narrowing of the airways. Smokers are at a higher risk of developing the chronic obstructive pulmonary disease (COPD) and lung cancer, both of which can lead to severe lung damage.
Environmental Factors
Exposure to environmental pollutants such as chemicals, dust, and air pollution can cause lung damage. Pollutants can irritate the airways and cause inflammation, leading to respiratory symptoms such as coughing, wheezing, and shortness of breath. People who work in industries with high levels of pollutants, such as mining and construction, may be at a higher risk of lung damage.
Respiratory Infections
Respiratory infections such as pneumonia, influenza, and COVID-19 can cause severe lung damage. Infections can cause inflammation and damage to the air sacs, leading to respiratory symptoms such as coughing, wheezing, and shortness of breath. In severe cases, respiratory infections can cause acute respiratory distress syndrome (ARDS), which can be life-threatening.
Genetics
Genetic factors can play a role in the severity of lung damage. People with genetic mutations such as alpha-1 antitrypsin deficiency may be at a higher risk of developing lung diseases, including COPD and emphysema.
Lifestyle Factors
Lifestyle factors such as diet and exercise can also impact the severity of lung damage. A healthy diet rich in fruits, vegetables, and whole grains can help reduce inflammation and promote lung health. Regular exercise can also improve lung function and reduce the risk of lung disease.
Read also:-
Why is Walking Considered the Best Exercise
Conclusion
While COVID-19 does not directly cause asthma, it can lead to respiratory symptoms that mimic asthma and trigger asthma symptoms in people who already have asthma. Understanding the link between COVID-19 and asthma is crucial for early diagnosis and treatment of respiratory symptoms. If you had COVID-19 and experience new or persistent respiratory symptoms, it is important to seek medical attention promptly.